
GENERAL SURGERY
LAPAROSCOPIC SURGERY

GASTROINTESTINAL SURGERY

MATERNITY SERVICES

INFERTILITY SERVICES

COSMETIC GYNECOLOGY
GENERAL SURGERY
General Surgery is a discipline of surgery having a central core of knowledge embracing anatomy, physiology, metabolism, immunology, nutrition, pathology, wound healing, shock and resuscitation, intensive care, and neoplasia, which are common to all surgical specialties.
Nine primary components of surgery are:
- Alimentary tract
- Abdomen and its contents
- Breast, skin, and soft tissue
- Head and neck, including trauma, vascular, endocrine, congenital and oncologic disorders - particularly tumors of the skin, salivary glands, thyroid, parathyroid, and the oral cavity
- Vascular system, excluding the intracranial vessels and heart
- Endocrine system, including thyroid, parathyroid, adrenal, and endocrine pancreas
- Surgical oncology, including coordinated multimodality management of the cancer patient by screening, surveillance, surgical adjunctive therapy, rehabilitation, and follow-up
- Comprehensive management of trauma, including musculoskeletal, hand, and head injuries. The responsibility for all phases of care of the injured patient is an essential component of general surgery.
- Complete care of critically ill patients with underlying surgical conditions, in the emergency room, intensive care unit, and trauma/burn units.

Open Breast Biopsy/Lumpectomy
Open breast biopsy is a procedure used when your doctor feels a lump. A needle-directed biopsy is used when the doctor cannot feel a lump, but there is an abnormality in the mammogram that warrants biopsy. Though the anesthesia is usually local (numbing medicine injected at the site of incision) with intravenous sedation, a short general anesthesia can also be used for uncooperative patients.
Core Breast Biopsy
The core breast biopsy helps doctors accurately diagnose breast abnormalities.It is performed in less than 1 hour, requires only a single ¼ inch incision, and requires no stitches. It is done in the office under local anesthesia.
This offers women an alternative to an open surgical biopsy, the most common biopsy method, which can leave scars and result in disfigurement of the breast. The procedure is performed using ultrasound guidance to allow greater accuracy in needle placement. Women are able to resume normal activity immediately following the procedure with only a small adhesive strip to cover the incision site.
Varicose Veins
Disorders of leg veins such as varicose veins or spider veins are extremely common. If a normal vein gets stretched out beyond its normal size, it will never return back to its original size. Once the normal vein is enlarged, it is very easy for it to continue to enlarge. If this vein is located under the skin it can grow to quite substantial in size and is termed a varicose vein. If it is a normally a small vein located within the skin, this is usually termed a spider vein. Both varicose veins and spider veins can form very large networks. As these veins enlarge they quite commonly become painful and symptomatic.
The causes of varicose veins and spider veins are commonly related to pregnancy, prolonged standing or walking, a previous deep vein clot, or even a hereditary disposition. Sometimes, a cause for varicose veins cannot be determined.
Treatment
Initially, treatment for enlarged veins of the lower extremities includes compression. This could be with elastic bandages or fitted compression stockings. Unfortunately, these treatments can be quite cumbersome and in warm weather can be uncomfortable.
Fortunately varicose veins and spider veins are easy to treat. Larger varicose veins can be treated with VNUS closure. This is an alternative to vein-stripping. This is often followed by ambulatory phlebectomy which removes the visible varicose veins under the skin. Finally, sclerotherapy is used for the spider veins in the skin.
Hemorrhoids
Hemorrhoids, one of the most common ailments in both men and women affect more than half the population at some point in their lives. Onset commonly occurs after the age of 30, but hemorrhoids are reported in people of all ages. More than 525,000 patients in the United States are treated annually for symptomatic hemorrhoids. Of these, approximately 10–20 percent will require surgical treatment for their condition.
Hemorrhoids are swollen veins. Veins around the anus tend to stretch under pressure, somewhat like varicose veins in the legs. When these veins swell, they are called “hemorrhoids.” One set of veins is inside the rectum (internal hemorrhoids) and another is under the skin around the anus (external hemorrhoids).
Internal Hemorrhoids
Internal hemorrhoids usually are not painful, but may bleed. Sometimes, an internal hemorrhoid may stretch until it bulges outside the anus. This is called a prolapsed hemorrhoid. A prolapsed hemorrhoid can go back inside the rectum on its own, or it can be gently pushed back inside. If the prolapsed hemorrhoid cannot be pushed back inside, consultation with a physician about surgical treatment options is necessary.
External Hemorrhoids
External hemorrhoids involve the veins outside the anus. They can be itchy or painful and can sometimes crack and bleed. If a blood clot forms, one may feel a tender lump on the edge of the anus, and see bright red blood on toilet paper or in the toilet after a bowel movement.
Symptoms of hemorrhoids, both external and internal, include aching after a bowel movement; anal or rectal itching; bright red blood on toilet tissue or in toilet bowl; appearance of anal tissue pads or sensitive lumps. When any of these symptoms are present, it is important to see a doctor to make sure the cause of the discomfort is hemorrhoids and not some other problem.
A person may be more likely to get hemorrhoids as they age or if their parents had them. Pregnant women often get hemorrhoids because of the strain from carrying the baby and from giving birth. For most women, such hemorrhoids are a temporary problem. Being over weight, straining to move your bowels, sitting too long on the toilet, or standing or lifting too much can make hemorrhoids worse. Constipation is the main cause of hemorrhoids.
Tips for hemorrhoid prevention:
- Include more fiber in your diet. Fresh fruits, leafy vegetables, and whole-grain breads and cereals are good sources of fiber.
- Drink plenty of fluids (except alcohol). Eight glasses of water each day is ideal.
- Do not read on the toilet. Sitting and straining too long encourages swelling.
- Exercise regularly.
- Avoid laxatives, except bulk-forming laxatives, such as Fiberall, Metamucil, etc. Other types of laxatives can lead to diarrhea, which can worsen hemorrhoids
- When you feel the need to have a bowel movement, don’t wait for long periods before using the bathroom.
Tips to reduce the pain caused by hemorrhoids:
- Take warm soaks three or four times a day.
- Clean your anus after each bowel movement by patting gently with moist toilet paper or moistened pads, such as baby wipes.
- Use ice packs to relieve swelling.
- Use acetaminophen (Tylenol®), ibuprofen (Motrin®), or aspirin to help relieve pain.
- Apply a cream that contains witch hazel to the area or use a numbing ointment. Creams that contain hydrocortisone can be used for itching or pain.
Treatment
Often lifestyle changes, topical medications, and good hygiene are all that is needed to reduce the symptoms of hemorrhoids. Most painful hemorrhoids stop hurting on their own in one to two weeks. If the pain persists, it is time to talk to a physician about other treatment options.
In a certain percentage of cases, surgical procedures are necessary to provide satisfactory, long-term relief. The newest procedure for advanced hemorrhoids is called the Procedure for Prolapse and Hemorrhoids (PPH). PPH is a technique that reduces the prolapse (enlargement) of hemorrhoidal tissue. With the PPH procedure, patients experience less pain and recover faster than patients who undergo the conventional hemorrhoidectomy procedure.
PPH reduces the prolapse of hemorrhoidal tissue by cutting out a band of the prolapsed anal mucosal membrane with the use of a circular stapling device. The PPH procedure essentially “lifts up” or repositions the mucosal, or anal canal tissue, and restores the hemorrhoidal tissue back to its original anatomical position. This reduces blood flow to the internal hemorrhoids. These internal hemorrhoids, then, typically shrink within four to six weeks after the procedure. The PPH procedure results in less pain than traditional procedures because it is performed above the “pain” line, or dentate line, inside the anal canal. The advantage is this method affects few nerve endings, while traditional procedures are performed below the dentate line, affecting many sensitive nerve endings.
For patients with a lesser degree of prolapse (internal hemorrhoids that have fallen outside the anus), rubber band ligation is widely used for the treatment of internal hemorrhoids. In this procedure, the hemorrhoidal tissue is pulled into a double-sleeved cylinder to allow the placement of latex/rubber bands around the tissue. Over time, the tissue below the bands dies-off and is eliminated during a bowel movement. Rubber band ligation can be performed in a doctor’s office and requires little preparation. Often, however, there is the need for more than one procedure to resolve a patient’s condition.
In cases involving a greater degree of prolapse, a variety of operative techniques are employed to address the problem. In traditional hemorrhoidectomy, surgery is used to remove the hemorrhoids. A hemorrhoidectomy removes excessive tissue that causes the bleeding or protrusion. It is done under anesthesia and may require hospitalization and a period of inactivity. Laser hemorrhoidectomies do not offer any advantage over standard operative techniques. They also are quite expensive, and contrary to popular belief, are no less painful.
Although anorectal conditions are benign and easily treated, patients may delay seeking medical advice because of embarrassment of hemorrhoids or fear of cancer. As a result, many patients first see their physician when the problem is advanced, requiring extensive treatment, and causing greater patient distress than if the conditions had been adequately diagnosed and managed at an earlier stage.
Procedure for Advanced Hemorrhoids (Involves Less Pain and a Quicker Recovery)
The Procedure for Prolapse and Hemorrhoids (PPH) eliminates the need for traditional hemorrhoidectomy for many patients. PPH is a technique that reduces the prolapse (enlargement) of hemorrhoidal tissue. With the PPH procedure, patients experience significantly less pain and recover faster than patients who undergo conventional hemorrhoidectomy procedures.
Results from PPH Clinical Trials
Compared to traditional hemorrhoidectomy, several studies have demonstrated that patients undergoing the PPH procedure:
- experienced significantly less pain
- experienced a quicker return to normal activities, including work
- spent less time in the hospital
- experienced less post-operative pain
- experienced less post-operative bleeding
- experienced less post-operative itching
- experienced less post-operative incontinence and constipation
How PPH Works
Using a stapling device, the PPH procedure essentially “lifts up” or repositions the mucosa, or anal canal tissue, and reduces blood flow to the internal hemorrhoids. These internal hemorrhoids, then, typically shrink within four to six weeks after the procedure. The PPH procedure results in less pain than traditional procedures because it is performed above the “pain” line, or dentate line inside the anal canal. The advantage is that this method affects few nerve endings, while traditional procedures are performed below the dentate line, affecting many sensitive nerve endings.
PPH Indications
PPH is indicated for patients with:
- Second degree hemorrhoids after failure of multiple rubber band ligation
- Third and fourth degree hemorrhoids
- Rectal mucosal prolapse
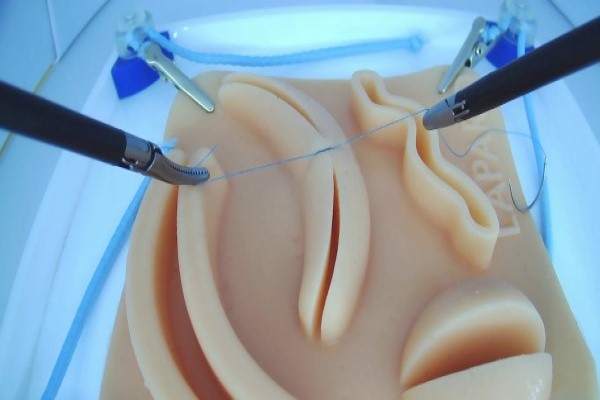
LAPAROSCOPIC SURGERY
A laparoscopy is a type of keyhole surgery that's performed in the abdominal (belly) area. It has advantages over traditional surgery, such as more rapid recovery, reduced pain and much smaller scars.
It requires special training. People who have keyhole surgery usually recover quite quickly.
Laparoscopy is keyhole surgery used to examine or operate on the interior of the abdominal or pelvic cavities. It is performed under general anaesthesia, usually by a surgeon or gynaecologist (women's health specialist).
During laparoscopy (also known as peritoneoscopy), a small cut is made in the abdomen. A thin tube containing a light and camera, known as a laparoscope, is then inserted to look inside the abdomen and pelvis. Gas is used to inflate the belly so the surgeon can see the organs properly.
One or more other small incisions may be made for other small instruments if needed.
Laparoscopy is used to diagnosis conditions or perform surgery in the abdominal and pelvic area. It can be used to:
- assess painful or heavy periods
- remove the uterus, fallopian tubes or ovaries
- diagnose or remove ovarian cysts
- assess female infertility
- treat ectopic pregnancy
- remove cysts or other tumours
- remove the gall bladder
- remove parts of the intestine
- take a biopsy (a small tissue sample) for testing
the causes of ongoing abdominal or pelvic pain.
After the procedure
When you wake from the procedure, you may feel a little sore around the cuts. You may also have some pain in your shoulder - this is caused by pressure from the gas in your abdomen.
After a few hours in recovery, you are likely to be sent home with care instructions, including about any pain, dressings and stiches you may have.
Laparoscopy complications
Like any surgery, laparoscopy can have complications such as:
- bleeding from the incisions
- infection
- damage to an organ or blood vessel.
As with any operation, there is also a small risk of complications associated with general anaesthesia.
Notify the hospital or your doctor immediately if you have:
- pain that is worsening or not improving
- increasing pain in your shoulders
- pain or other problems when urinating
- bleeding that is increasing or not settling
- a fever or temperature
- you feel that you are not recovering relatively quickly
- any other symptoms that you are concerned about.
Laparoscopic Cholecystectomy
Removal of the gallbladder is a very common procedure as about 600,000 gallbladders are removed in the United States every year! The gallbladder is responsible for storage of a small amount of bile for use after a fatty meal. However, when the gallbladder gets stones that have formed, it will often get symptoms of pain and bloating. These are signs that more serious complications such as infection and bile duct blockage may also occur. The vast majority of gallbladders are removed with the laparoscope.
Laparoscopic Nissen Fundoplication
Nissen Fundoplication is used in patients with gastroesophageal reflux disease (GERD). During the operation the top part of the stomach, called the fundus, is wrapped around the area where the esophagus meets the stomach. This will tighten the sphincter muscle that is between the esophagus and stomach and allow this sphincter to function properly again. The entire operation can be done with the laparoscope.
Nearly every patient can go home the day after the operation.
Recent data suggests that this operation will help in some patients to cause regression of Barrett’s esophagus which is a precancerous change in the lining of the lower esophagus.
This operation is also beneficial not only for those patients who have stopped responding to medical therapy for GERD but also for patients who are relatively healthy and do not want to take a lifetime of antacid medication. The vast majority of patients after this operation do not need supplementation with antacids or acid suppression pills.
Laparoscopic Ventral Hernia Repair
Ventral hernias are repaired on an elective basis to avoid internal organs getting stuck in the hernia. This can result in strangulation, or death of the internal organ.Every hernia is repaired with mesh when we use the laparoscope. This mesh is made of PTFE which is the material used in Gore-Tex™. The advantage of mesh is a more durable repair and less post-operative pain than the older type of hernia repair without mesh. Recurrence rates for a mesh repair are around 1% compared to around 10% with the older technique. This procedure is doen under general anesthesia.
Laparoscopic & Open Inguinal Hernia Repair
Inguinal (groin) hernias are repaired on an elective basis to avoid internal organs getting stuck in the hernia. This can result in strangulation, or death of the internal organ.Almost every hernia is repaired with mesh. This is woven polypropylene, or a type of plastic. The advantage of mesh is a more durable repair and less post-operative pain than the older type of hernia repair without mesh. Hernia repairs are performed laparoscopically when possible.
Laparoscopic Colon Resection
Segments of the colon or the entire colon can be removed utilizing the laparoscope for a “minimally invasive” approach. The laparoscopic portion of the operation is performed with the aide of a scope in a ½” incision around the umbilicus (belly button). The position of other incisions, or ports, is dependent on the specific operation that is performed. Your surgeon will give you specific details about incision locations at your preoperative appointment.
Another new innovation that our surgeons use is called the hand assist technique. This is used for difficult operations that could not normally be done using the laparoscope. It allows the surgeon to put his hand in the abdomen through a small incision while the remainder of the operation is done laparoscopically. This allows the best of both open and laparoscopic surgery.
The advantage to laparoscopic or hand-assisted laparoscopic surgery is quicker recovery time and shorter hospital stay. We have found that the length of hospital stay has shortened to 1-3 days for laparoscopic colon resection as compared to 3-5 days for the traditional open operation. This is primarily because the post-operative pain is much less and fewer narcotics are used for pain control in the post-operative period.
We generally do not perform laparoscopic colon resection for colon cancer because the scientific data is not there to support that the cancer survival rate is the same as with an open operation. In the near future, we expect the data to support laparoscopic resections for cancer and we will then change our practices accordingly.
GASTROINTESTINAL SURGERY
What is gastrointestinal surgery?
Gastrointestinal surgery is a treatment for diseases of the parts of the body involved in digestion. This includes the esophagus (ee-sof-uh-gus), stomach, small intestine, large intestine, and rectum. It also includes the liver, gallbladder, and pancreas.
Surgery may be used to remove a cancerous or noncancerous growth or damaged part of the body, such as the intestine. It may also be used to repair a problem like a hernia (a hole or weak spot in the wall of the abdomen). Minor surgical procedures are used to screen and diagnose problems of the digestive system.

Below are gastrointestinal conditions that may be treated with surgery:
- Appendicitis. When the appendix becomes infected and inflamed, it may be removed (appendectomy).
- Colon cancer and other gastrointestinal cancers. Surgery is done to remove cancerous tumors in the digestive system and parts of the digestive system that have cancer. For example, a surgeon may remove a tumor as well as part of the pancreas, liver, or intestine with cancer.
- Diverticular disease. A diverticulum is a small pouch or pocket in the colon (large intestine). Researchers are not sure why these develop. Sometimes they can become inflamed and cause pain (diverticulitis). This is often managed without surgery. If someone has a lot of diverticula that often become inflamed, the doctor may recommend bowel resection surgery to remove that part of the intestine.
- Gallbladder disease. When there is a problem with the gallbladder — usually gallstones — the gallbladder can be removed. Surgery to remove the gallbladder is also called a cholecystectomy (koh-luh-si-stek-tuh-mee).
- Gastroesophageal reflux disease (GERD) and hiatal hernias. GERD, or acid reflux is when the acid from the stomach backs up into the esophagus (food pipe) and causes heartburn. Sometimes it happens because of a hiatal hernia. This is when the stomach pushes through the diaphragm, a muscle that separates the chest from the abdomen. A surgeon can do a surgery called fundoplication (fun-doh-pluh-cay-shun) to fix it. The surgeon will fix the hernia if there is one and then wrap the top of the stomach around the bottom of the esophagus to strengthen the sphincter, which keeps acid out.
- Hernia. A hernia is when a part of the body (like the intestine) comes through a hole or weak spot in the wall of muscle or connective tissue that’s supposed to protect it (like the abdomen). It doesn’t come through the skin, but a bulge may be felt under the skin that’s not supposed to be there. It can also be painful. Gastrointestinal surgeons can repair the hole or weak spot.
- Inflammatory bowel disease (Crohn’s disease and ulcerative colitis). With inflammatory bowel disease, the immune system attacks the intestines and causes pain and inflammation. This can lead to damage in the intestine. Sometimes the damaged parts are removed and the healthy parts are reconnected. This is called bowel resection.
- Rectal prolapse. Surgery is used to treat rectal prolapse, a condition in which part of the intestine comes through the anus.
- Weight loss. Different types of bariatric surgery (for example, gastric bypass) may be done to treat obesity. This surgery is usually done by a specialist in bariatric surgery.
A surgical procedure called an endoscopy is used to screen and diagnose problems of the digestive system. The doctor puts a long, thin tube with a tiny camera into the body to see inside. If the problem is with the stomach or esophagus, the doctor puts the scope through the esophagus. To check for colon cancer or other problems of the intestines, the doctor puts the scope through the anus into the intestine.
MATERNITY SERVICES
Respectful maternity care – refers to care organized for and provided to all women in a manner that maintains their dignity, privacy and confidentiality, ensures freedom from harm and mistreatment, and enables informed choice and continuous support during labour and childbirth .
Kamala women’s hospital provides an up-to-date structure for the delivery of quality and safe maternity care as recommended by WHO. We cover:
- Pre-pregnancy services
- Antenatal care
- High risk pregnancy
- Inpatient care
- Elective birth
- Intrapartum care
- Postnatal care

INFERTILITY SERVICES
Infertility evaluation can be expensive, and sometimes involves uncomfortable procedures. Many medical plans may not reimburse the cost of fertility treatment. Finally, there's no guarantee — even after all the testing and counseling — that you'll get pregnant. Kamla hospital provides you with basic level 1 infertility services and for advanced procedure has tie up with other IVF centres.
Tests for men
Male fertility requires that the testicles produce enough healthy sperm, and that the sperm is ejaculated effectively into the woman's vagina and travels to the egg. Tests for male infertility attempt to determine whether any of these processes are impaired.
You may have a general physical exam, including examination of your genitals. Specific fertility tests may include:

- Semen analysis. Your doctor may ask for one or more semen specimens. Semen is generally obtained by masturbating or by interrupting intercourse and ejaculating your semen into a clean container. A lab analyzes your semen specimen. In some cases, sperm may be tested for in the urine.
- Hormone testing. You may have a blood test to determine the level of testosterone and other male hormones.
- Genetic testing. Genetic testing may be done to determine whether there's a genetic defect causing infertility.
- Testicular biopsy. In select cases, a testicular biopsy may be performed to identify abnormalities contributing to infertility and to retrieve sperm to use with assisted reproductive techniques, such as IVF.
- Imaging. In certain situations, imaging studies such as a brain MRI, bone mineral density scan, transrectal or scrotal ultrasound, or a test of the vas deferens (vasography) may be performed.
- Other specialty testing. In rare cases, other tests to evaluate the quality of the sperm may be performed, such as evaluating a semen specimen for DNA abnormalities.
Tests for women
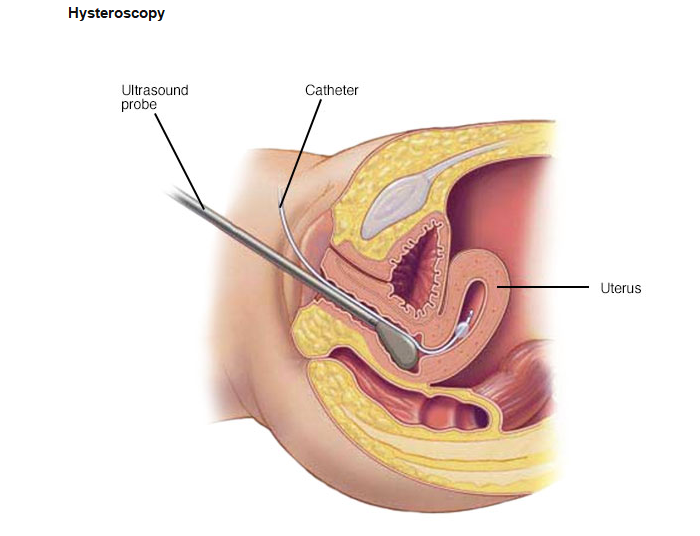
Sonohysterography
Fertility for women relies on the ovaries releasing healthy eggs. Her reproductive tract must allow an egg to pass into her fallopian tubes and join with sperm for fertilization. The fertilized egg must travel to the uterus and implant in the lining. Tests for female infertility attempt to determine whether any of these processes are impaired.
You may have a general physical exam, including a regular gynecological exam. Specific fertility tests may include:
- Ovulation testing. A blood test measures hormone levels to determine whether you're ovulating.
- Hysterosalpingography. Hysterosalpingography (his-tur-o-sal-ping-GOG-ruh-fee) evaluates the condition of your uterus and fallopian tubes and looks for blockages or other problems. X-ray contrast is injected into your uterus, and an X-ray is taken to determine if the cavity is normal and ensure the fluid spills out of your fallopian tubes.
- Ovarian reserve testing. This testing helps determine the quality and quantity of the eggs available for ovulation. This approach often begins with hormone testing early in the menstrual cycle.
- Other hormone testing. Other hormone tests check levels of ovulatory hormones, as well as pituitary hormones that control reproductive processes.
- Imaging tests. Pelvic ultrasound looks for uterine or fallopian tube disease. Sometimes a hysterosonography (his-tur-o-suh-NOG-ruh-fee) is used to see details inside the uterus that are not seen on a regular ultrasound.
Depending on your situation, rarely your testing may include:
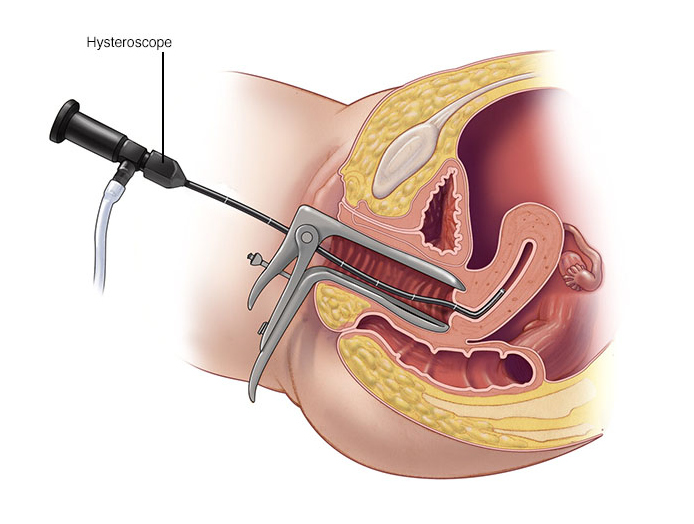
- Hysteroscopy. Based on your symptoms, your doctor may request a hysteroscopy to look for uterine or fallopian tube disease. During hysteroscopy, your doctor inserts a thin, lighted device through your cervix into your uterus to view any potential abnormalities.
- Laparoscopy. This minimally invasive surgery involves making a small incision beneath your navel and inserting a thin viewing device to examine your fallopian tubes, ovaries and uterus. A laparoscopy may identify endometriosis, scarring, blockages or irregularities of the fallopian tubes, and problems with the ovaries and uterus.
- Genetic testing. Genetic testing helps determine whether there's a genetic defect causing infertility.
Not everyone needs to have all, or even many, of these tests before the cause of infertility is found. You and your doctor will decide which tests you will have and when.
CANCER AND INFERTILITY
A very real and unfortunate side effect of cancer and cancer treatment is infertility. Various types of cancer and cancer treatments may have different effects on a woman’s fertility. Talk with your physician about the common side effects of your specific cancer type, as well as the effects of various treatments. Keep in mind that timing may play a crucial role in preserving fertility and that your doctor may recommend immediate action depending upon the severity of your diagnosis.
TREATMENT RISKS
Chemotherapy
Cancer treatment with chemotherapy may affect fertility. The effects of chemotherapy for women depend on: age, drug type, drug quantity, and length of treatment.
Women who receive chemotherapy may have a change in their periods or menstrual cycles. Periods may become irregular, and flow may decrease or stop. Some women develop symptoms of menopause such as vaginal dryness and hot flashes. Younger women may have irregular periods during chemotherapy and may resume normal periods following treatment. Women who resume normal cycles after treatment may still be at risk for early menopause as their egg supply may have been damaged. Women over 40 are more likely to go into menopause immediately after treatment, which means they will never resume their cycle.
Radiation Therapy
Radiation to the pelvis or area of the reproductive organs can damage or destroy reproductive tissues and cells. This damage may be permanent or just temporary. As with chemotherapy, hormones are sometimes given along with treatment to improve the chances of having children once treatment is complete. Again, the administration of hormones may have negative effects on certain kinds of cancer.
Surgery
Some cancer surgeries may affect a woman’s ability to have a child. Speak with your physician about how a specific procedure may affect your fertility and ability to carry a baby.
FERTILITY OPTIONS
Fortunately, there is hope for pregnancy depending on the type and extent of cancer. Below are several options for women facing cancer-related infertility.
Embryo Freezing
Currently, embryo freezing is the most widely available and most standard practice. CCRM offers embryo freezing to patients with certain types of cancer. This procedure involves removing mature eggs during in vitro fertilization (IVF), combining them with partner or donor sperm in the laboratory, freezing, and then storing them. In standard IVF, eggs are matured through the use of hormone therapy. Because of the effects of hormones on certain types of cancer, embryo freezing is not an option for all cancer patients.
The embryo freezing process typically takes between 4-6 weeks and is available for women after puberty. Embryos may be stored until the cancer is in successful remission.
Your physician will let you know when it is safe to attempt pregnancy after cancer treatment. Once a patient has the approval of her physician, a CCRM physician will continue the IVF process by removing a limited number of frozen embryos from storage and implanting them into the patient’s uterus. Although there is no guarantee of pregnancy, CCRM consistently achieves some of the highest pregnancy success rates from IVF in the U
Egg Freezing
Egg freezing may be another viable option. During this process, unfertilized eggs are removed, frozen and stored for use at a later time. The procedure is similar to embryo freezing and requires the use of hormone therapy. Because of the effects of hormones on certain types of cancer, egg freezing is not an option for all cancer patients.
The egg freezing process typically takes two to six weeks and is available for women after puberty. Eggs may be stored until the cancer is in successful remission.
Embryo Transfer with Donor Eggs
In the event that a woman’s ovarian function is diminished as a result of chemotherapy or radiation, she may have the option of embryo transfer using donor eggs. During this procedure, a known or anonymous donor contributes eggs to be combined with a partner’s sperm. The fertilized embryo is then transferred into the patient’s uterus in an attempt at pregnancy.
COSMETIC GYNECOLOGY
We are specialists who address women’s functional and anatomical changes to the pelvic floor as a result of childbirth, aging, and other factors. Many of these women – our patients who we see daily – also complain of changes in sexual function and genital aesthetic appearance. We are genuinely fulfilling our duty as pelvic floor specialists to understand these concerns and regularly treats them .
Cosmetic Gynecology has become one of the fastest growing subspecialties of elective surgery for women includes both cosmetic procedures to enhance the aesthetic appearance of the vulvo/vaginal region, as well as functional vaginal repairs to enhance or help restore sexual function following the changes that may occur following childbirth and/or aging.
